Spinal/Subarachnoid Block
Angela Mordecai, DNP, CRNA and Bailey Freeman, DNP, CRNA
Quick Facts
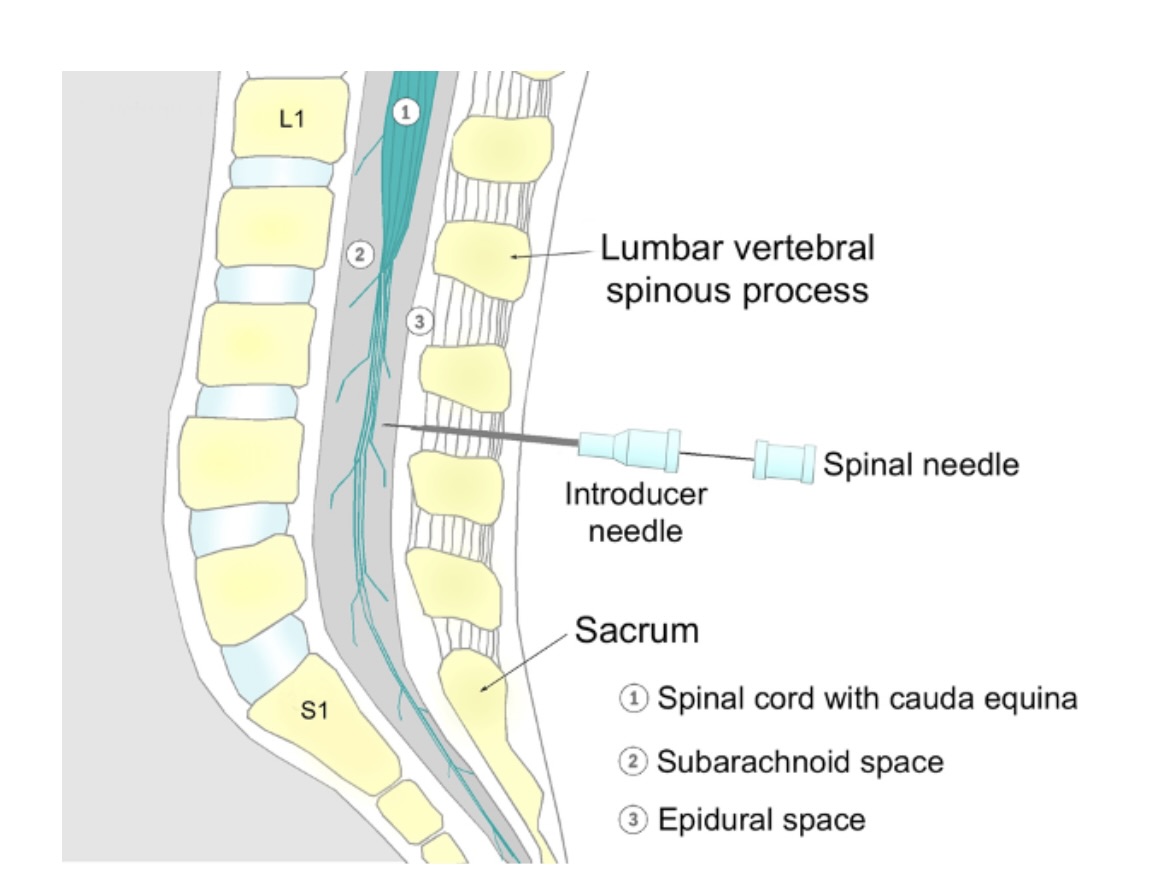
- The subarachnoid block, also known as a “spinal block,” is a form of neuraxial anesthesia that provides a temporary loss of sensation to the lower abdomen and lower extremities.
- The procedure involves the injection of local anesthetic into the subarachnoid space, where it exerts its effects on the spinal cord and nerve roots.
- Often, adjunctive medications are administered in combination with the local anesthetic for a synergistic effect. These medications may extend the duration of the block and/or provide additional analgesic properties.
- Subarachnoid blocks avoid many of the complications of general anesthesia such as ventilator-related issues, drowsiness, and postoperative nausea and vomiting.
- Subarachnoid blocks are the anesthetic method of choice for cesarean delivery because they avoid systemic circulation of medications and allow the mother to be awake for the birth.
- The patient may remain awake, or be sedated for anxiolysis.
- Generally, subarachnoid blocks last for 2 to 4 hours.
Indications
Subarachnoid blocks are indicated for various surgical procedures where regional anesthesia is preferred.
- Cesarean section
- Gynecological surgeries
- Urological surgeries
- Inguinal hernia repairs
- Orthopedic surgeries
- Hip replacements
- Knee replacements
- Lower extremity fracture repairs
- Ankle surgeries
Absolute Contraindications
- Patient refusal
- Allergy to local anesthetic
- Infection at the site of placement
- Elevated intracranial pressure
- Severe coagulopathy
- Severe aortic stenosis
- Pre-existing spinal cord damage
Relative Contraindications
- History of spinal surgery
- Spinal stenosis
- Aortic stenosis
- Anticoagulants
- Certain neurological disorders
- Inability to maintain position for the procedure
Procedure
Equipment Needed:
- Sterile spinal kit
- Introducer needle
- Spinal needle
- Filter needle
- Local infiltration (1% Lidocaine)
- Preservative-free spinal anesthetic solution (0.75% Bupivacaine w/ dextrose 8.25%), or choice of spinal local anesthetic
- Epinephrine 1%
- Antiseptic skin solution
- Sterile syringes, gauze, sponges, and drape
- Mayo stand
- Sterile gloves
Technique [add video]
- Apply monitors (SpO₂, NIBP, ECG)
- Apply 2L O₂ via NC
- Assist patient in sitting neuraxial position
- Prepare for procedure
- Using sterile technique, open spinal kit on mayo stand
- Apply sterile gloves
- Clean the back with sterile betadine solution (allow drying time)
- Draw up lidocaine and attach a 25g needle
- Draw up a height-based dose of bupivacaine (or other intended local anesthetic) along with any adjunct medications
- Place a sterile drape with an opening around the block placement site
- Position patient on the side of the bed, rounding the back out in a “mad cat” or “shrimp” position
- Locate the iliac crests and palpate the vertebral interspaces
- Mark the intended insertion site (often L3–4 or L4–5)
Block placement
*Always brace your left hand on the patient’s back to secure needle position
- Perform local anesthetic skin wheel (with about 2 ml of 2% lidocaine) at the block placement site
- Place the introducer needle, advancing slightly cephalad
(depth will depend on patient size; be careful not to breach the dura) - Place the spinal needle through the introducer and advance through the layers of tissue:
- Subcutaneous tissue
- Supraspinous ligament
- Intraspinous ligament
- Ligamentum flavum
- Dura
- Remove the stylet to observe for CSF
- Connect the spinal anesthetic syringe to the spinal needle and draw back slightly, assessing for a CSF “swirl”
- Slowly inject the spinal anesthetic solution
- May draw back to reassess for a “swirl” as a final confirmation of correct location
- Remove the introducer, spinal needle, and syringe in one single unit
- Assist patient into supine position (with left uterine displacement if pregnant)
Confirmation Steps
- Assure CSF is actively dripping before connecting the syringe with local anesthetic
- Aspirate before, during, and after injection to ensure accurate placement
- Once the patient is flat, test the sensory level with a blunt-tip cannula (“pinprick”) or cold object/alcohol swab
- Goal: Sensory block at least 2–3 dermatome levels above the operative site
Documentation Requirements
- Spinal kit lot number and expiration date
- Sterile measures taken
- Patient position during and after block placement
- Level of block placement
- Number of attempts
- Needle types used
- Level of sensory blockade obtained
- Any complications
SCOPE GUIDE
Strategies
- Review patient labs, with particular attention to WBC count and platelet count, which may indicate infection or coagulopathy.
- Spinals can be performed in the sitting or lateral side-lying positions.
- Sitting is more common as it is easier to place midline.
- Patient must be educated on the procedure and required positioning.
- Patient must be able to maintain the necessary position without moving during placement.
Clinical Optimization
- If the patient is on blood thinners, refer to the neuraxial anticoagulant protocol to ensure appropriate timing since the last dose.
- In anticipation of neuraxial-induced vasodilation, the patient should be fluid optimized prior to placement.
- Evidence suggests that co-loading fluid during the procedure, rather than preloading, is beneficial.
- Administer 1 L of crystalloid; consider 250–500 ml colloid.
- Giving ondansetron prior to the subarachnoid block may help prevent hypotension caused by the Bezold-Jerisch reflex.
- Anxiolysis may assist the patient in assuming and maintaining the required position.
- This may be achieved with 1–2 mg IV midazolam, precedex, or an IV narcotic.
- Sodium Bicitra should be given prophylactically in anticipation of nausea associated with a drop in SVR.
- Bicitra neutralizes stomach pH and reduces the risk of aspiration pneumonitis.
- Note baseline vitals and ensure they remain within 20% throughout the case.
- In very obese patients, a longer spinal needle may be required to access the space.
Pearls
Preparation
- Have a trash can nearby to discard supplies such as betadine sponges.
- Before donning sterile gloves, elevate the table so that the insertion site is at chest level.
- It is helpful to have an assistant for drawing up adjunctive medications such as fentanyl or duramorph.
Technical Considerations
- If having trouble accessing the spinal space, ensure proper positioning.
- The patient may need to round out their back further to allow maximal spreading of the spinous processes.
- Ask the patient if they feel insertion pressure on one side; a slight offset from midline may direct the needle out of range.
- Generally, start at the lower end of the intervertebral space and advance slightly cephalad.
- If osseous tissue obstructs needle advancement, pull back and redirect until the needle advances smoothly.
Managing Complications
- Hypotension: due to reduction in SVR
- Have Neosynephrine and Ephedrine readily available.
- Ensure IV fluids are infusing wide open.
- Consider colloid infusion.
- Bradycardia: may occur due to sympathetic blockade (T1–4)
- Ephedrine 5–10 mg
- Glycopyrrolate 0.2 mg
- Atropine 0.4 mg
- Nausea/Vomiting
- Sodium Bicitra should be given prior to block placement.
- Zofran (dose per provider discretion) given before or shortly after placement.
- Additional antiemetics (decadron, reglan, or phenergan) as needed.
- High Spinal *EMERGENCY*: Patient may lose the ability to breathe*This may occur if the local anesthetic dose is too high or administered too quickly.
- Support ventilation with bag/mask if not contraindicated.
- If the patient is pregnant or has a full stomach, induce general anesthesia and intubate.
- Administer midazolam promptly for anxiolysis.
- The patient may need to remain sedated and ventilated until respiratory effort resumes.
- Spinal/Post-Dural Puncture (PDPH) Headache:*May occur due to excessive CSF loss from multiple attempts or a larger gauge needle. Symptoms may begin immediately or within 24–48 hours. Headache worsens when upright and improves when supine.
- Spinal Hematoma: Rare complication (<1:150,000)
- Typically a complication of coagulopathy during placement; may result in permanent nerve injury.
- Prevention is key—review preoperative lab values carefully.
- Follow neuraxial protocols for patients on anticoagulants.
- Treatment may include steroids, anti-inflammatories, or surgical decompression in severe cases.
- Meningitis/Infection
- May lead to neurological injury.
- Strict sterile technique is essential to prevent this complication.
- Treatment depends on the causative organism (antibiotics or antivirals).
Quick Resources
References
1. Hocking G. Assessment of spinal anaesthetic block. WFSA Resource Library. Published October 12, 2009. https://resources.wfsahq.org/atotw/assessment-of-spinal-anaesthetic-block/
2. Barash PG, Cullen BF, Stoelting RK, et al. Clinical Anesthesia. 8th ed. Wolters Kluwer; 2017.
3. SUBARACHNOID BLOCK (ALSO KNOWN AS SPINAL BLOCK). WFSA Resource Library. https://resources.wfsahq.org/atotw/subarachnoid-block-also-known-as-spinal-block/
Media Attributions
- Spinal

