Principles of Airway Management
Bailey Freeman, DNP, CRNA; Angela Mordecai, DNP, CRNA; Brian Cornelius, DNP, CRNA; and Kristin Barkley, DNP, CRNA
Quick Facts
Airway Assessment (Anesthesia-Focused)
Risk Factors for Difficult Airway
Airway Emergencies (Introduced)
Introductory Techniques
Confirmation & Monitoring
Team, Equipment & Preparation
Scope Guide
Airway Assessment (Anesthesia-Focused)
Risk Factors for Difficult Airway
Airway Emergencies (Introduced)
Introductory Techniques
Confirmation & Monitoring
Team, Equipment & Preparation
Scope Guide
Quick Facts
- Airway management aims to maintain patency and ensure adequate oxygenation/ventilation through positioning, maneuvers, adjuncts, and definitive devices.
- A structured pre-anesthesia airway assessment helps predict difficulty and guides backup planning.
- Mask ventilation is the cornerstone rescue; supraglottic devices and endotracheal intubation provide escalating control of the airway.
Airway Assessment (Anesthesia-Focused)
Perform and document these elements on every patient before anesthesia or procedural sedation:
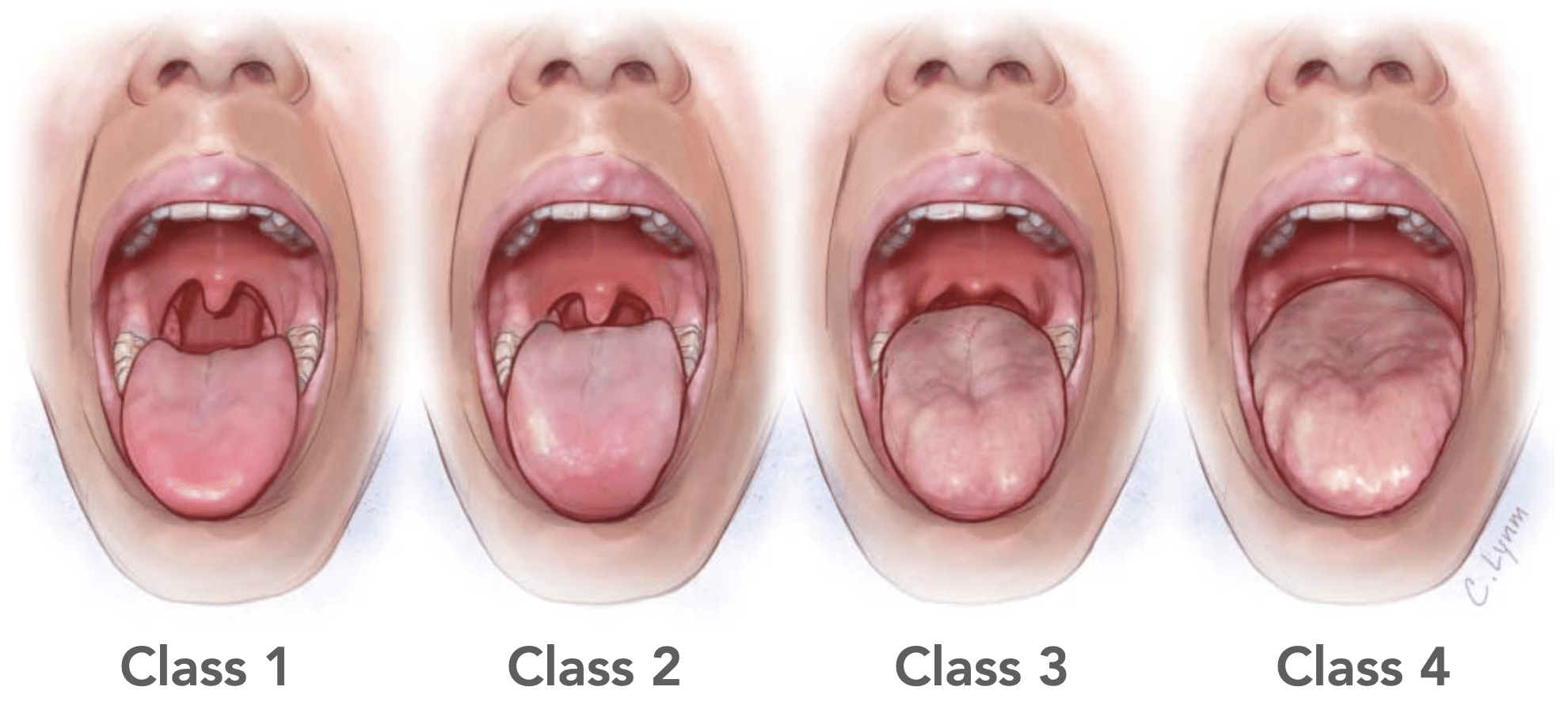
- Mallampati Classification (I–IV): Patient seated, mouth open, tongue protruded, no phonation. Higher classes (III–IV) suggest more difficult laryngoscopy and may correlate with mask difficulty.
- Inter-Incisor Gap / Mouth Opening: Normal >3 cm (~2–3 fingerbreadths). Limited opening complicates laryngoscopy, LMA insertion, and adjunct placement.
- Upper Lip Bite Test: Mandibular protrusion capacity (Class I–III). Class III can predict difficult laryngoscopy.
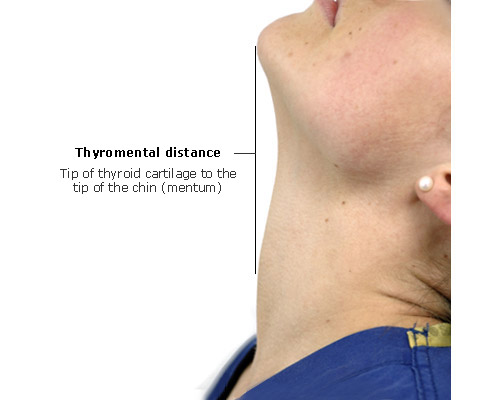
- Thyromental Distance: >6.5 cm (~3 FB) is typical; shorter distance implies reduced mandibular space and more challenging visualization.
- Hyomental Distance: Assesses submandibular space; reduced distance may predict difficulty.
- Neck Circumference: Larger circumference (e.g., >43 cm) increases risk of difficult mask ventilation/intubation, especially with obesity.
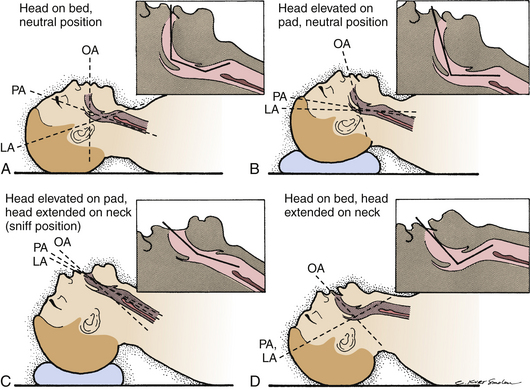
- Cervical Spine Range of Motion: Flexion/extension/rotation. Limited extension impairs alignment of airway axes.
- Dentition: Prominent incisors, loose/chipped teeth, edentulism (each has distinct implications for mask seal and laryngoscopy).
- History: Snoring/OSA, prior difficult airway, radiation/neck mass, facial hair, trauma or prior airway surgery.
- Physiology: Anticipate reduced apneic time in pregnancy, obesity, pediatrics, and critical illness.
Risk Factors for Difficult Airway
- Difficult Mask Ventilation: Age >55, male sex, higher BMI/obesity, facial hair, edentulism, Mallampati III–IV, snoring/OSA, limited jaw protrusion, increased neck circumference, prior neck irradiation.
- Difficult Supraglottic Airway: Limited mouth opening, poor dentition, high BMI, restricted neck mobility.
- Difficult Laryngoscopy/Intubation: Mallampati III–IV, short thyromental distance, limited cervical extension, micrognathia/retrognathia, prior difficult airway, airway mass/radiation.
- High-risk Combination: Difficult mask ventilation with difficult laryngoscopy is uncommon but high-stakes; plan early backups.
Airway Emergencies
- Obstruction: Tongue collapse, secretions, edema, mass, foreign body, external compression. Clues: paradoxical or absent airflow, stridor, snoring, desaturation.
- Laryngospasm: Reflex glottic closure (often during induction/emergence). Clues: stridor, retractions, inability to ventilate. Requires immediate maneuvers and deepening/relaxation strategies (covered here).
- Bronchospasm: Lower-airway constriction; clues include wheeze, rising airway pressures, prolonged expiration, EtCO₂ “shark fin.” Manage with bronchodilation and optimized ventilation (covered here).
Introductory Techniques
- Mask Ventilation: Ensure oxygen flow, proper mask size/position, and an effective seal (one-hand C–E or two-hand technique). Use jaw thrust/chin lift and adjuncts (OPA/NPA) as needed. Keep pressures ≤20 cmH₂O to limit gastric insufflation.
- Supraglottic Airway (e.g., LMA): Rapid rescue/primary airway above the cords. Choose size, insert along the palate, inflate cuff per device recommendations, and confirm ventilation. Useful bridge when intubation is delayed or difficult.
- Endotracheal Intubation (brief): Direct or video laryngoscopy to pass an ETT through the cords; standard for aspiration protection and controlled ventilation. Select size, blade (Mac/Miller), and plan RSI when indicated. Confirm with waveform capnography.
Confirmation & Monitoring
- Waveform Capnography: Continuous ETCO₂ is the most reliable confirmation of ventilation and ETT placement (sustained waveform).
- Pulse Oximetry: Oxygenation status; lagging indicator during rapid desaturation.
- Clinical Exam: Chest rise, auscultation, mist in circuit, no epigastric insufflation.
- Assessment: Ultrasound and chest X-ray can support confirmation and depth (ETT ~2 cm above carina after head/neck neutralization).
Equipment & Preparation
- Equipment: O₂ source, suction, mask + circuit, OPA/NPA, LMA’s, laryngoscope(s) (direct/video), ETTs + bougie/stylet, capnography, securing materials.
- Preparation: Preoxygenate; choose induction/neuromuscular agents; apply in-line stabilization if trauma; understand device contraindications (e.g., OPA with intact gag; caution with NPA and midface/basal skull trauma).
Scope Guide
Strategies
- Perform a full anesthesia airway assessment and document risk factors.
- Always have a back up plan.
- And a back up to the back up plan.
- Call for help sooner than later
Clinical Optimization
- Position (head-elevated sniffing when safe)
- Use adjuncts for difficult ventilation: mask straps, two-handed technique with ventilator turned on, two-person mask technique
- Use adjuncts for difficult intubation: bougie, video laryngoscopy
- If can’t ventilate/can’t intubate → LMA
Pearls
- Mallampati is only one piece of the puzzle; integrate mouth opening, TMD, ROM, dentition, neck circumference, and history.
- Mask ventilation skill is lifesaving; inability to ventilate is more often a seal/position issue than a need for immediate intubation.
- Call for help when needed!
- See Sniffing Position in Diagram C:
References
- Bradley WPL, Lyons C. Facemask ventilation. BJA Education. 2022;22(1):5–11.
- Baker P. Mask ventilation. F1000Res. 2018;7:F1000 Faculty Rev-1580. PMCID: PMC6206602.
- Yildiz TS, Solak M, Toker K. Incidence and risk factors of difficult mask ventilation. Can J Anesth. 2005;52(8):873–879.
- Avva U, Lata JM, Hendrix JM, Kiel J. Airway Management. StatPearls. Updated Jan 19, 2025.
- Simulation Two handout (program educational material): Airway evaluation, mask ventilation, and intubation.
Media Attributions
- Mallampati-classification-JAMA-2013
- ana_1_030_12_t1_01_med
- B9781416037736100497_gr6

