Anaphylaxis
Kristin Barkley, DNP, CRNA
Anaphylaxis
- Estimated frequency: ~1 in 3,500–20,000 anesthetized patients.
- ~60–70% are IgE-mediated Type I reactions.
- Neuromuscular blocking drugs are the most common drug class implicated.
- Succinylcholine and rocuronium are the most frequently involved NMBAs.
Types of Hypersensitivity Reactions
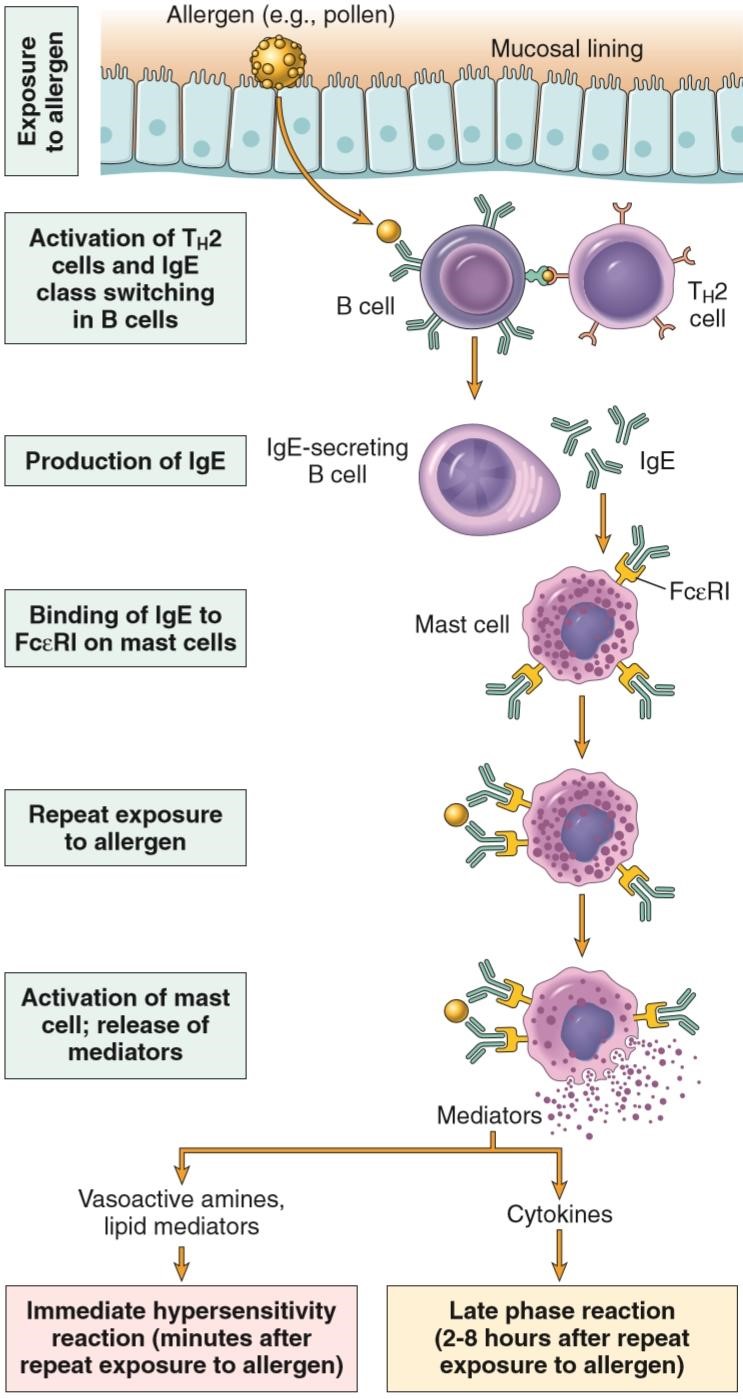
Type I — Anaphylactic/Immediate
- Mediator: IgE
- Examples: drug allergy, hay fever, asthma, hives
Type II — Cytotoxic
- Mediators: IgG, IgM, complement
- Examples: blood transfusion reactions, acute transplant rejection
Type III — Immune Complex
- Mediators: IgG, IgM, neutrophils, complement
- Examples: systemic lupus erythematosus, rheumatoid arthritis
Type IV — Delayed (Cell-mediated)
- Mediators: T cells, monocytes/macrophages, cytokines
- Examples: poison ivy, transplant rejection
Type V — Stimulatory
- Mediator: humoral antibodies
- Example: Graves’ disease
SCOPe Guide
Strategies
Recognition (Grading)
- Grade I: cutaneous signs — generalized erythema, urticaria, angioedema.
- Grade II: Grade I + hypotension, tachycardia, cough, difficult ventilation.
- Grade III: hypotension, tachycardia/bradycardia, arrhythmias, bronchospasm.
- Grade IV: cardiac and/or respiratory arrest, pulseless electrical activity.
Treatment
- Stop suspected trigger.
- Position: Trendelenburg to improve venous return.
- Ventilation: ensure 100% O2.
- Manage hypotension — Epinephrine is first-line:
- Grade II: 10–20 mcg SC/IM.
- Grade III: 100–200 mcg SC/IM/IV every 1–2 minutes as needed.
- Grade IV: 1 mg IV; repeat per ACLS.
- Secondary vasopressor: Vasopressin 2–10 units IV if needed.
- Refractory vasoplegia: Methylene blue (inhibits guanylate cyclase → ↓cGMP) may be considered.
- Fluids: Crystalloid 10–30 mL/kg or colloid 10 mL/kg.
- Bronchospasm: Albuterol or ipratropium inhalers; Terbutaline 0.25 mg SC.
- Antihistamines:
- H1: Diphenhydramine or Hydroxyzine 0.5–1.0 mg/kg IV.
- H2: Ranitidine 50 mg IV or Famotidine 20 mg IV.
- Airway edema / inflammation: Steroids are adjuncts (not immediate effect).
- Hydrocortisone 250 mg IV.
Clinical Optimization
- Presentation under anesthesia: cutaneous signs may be obscured by drapes; watch for hypotension, tachycardia, bronchospasm → hypovolemia, shock, hypoxemia → arrest.
- Pathophysiology: re-exposure → IgE cross-linking on mast cells/basophils → degranulation → mediator release:
- Histamine: vasodilation, ↑permeability (edema/urticaria), pulmonary edema.
- Leukotrienes: bronchoconstriction, ↑permeability.
- Prostaglandin D2: bronchoconstriction.
- Platelet-activating factor: bronchoconstriction, ↑permeability.
- Epinephrine is primary:
- Stabilizes mast cells/basophils (↓degranulation).
- α1/β1: ↑BP and inotropy; β2: bronchodilation.
Pearls
- Rapid recognition and treatment prevent progression and refractory shock.
- Epinephrine first, then fluids and adjuncts.
- Consider timing: immediate after IV drug vs delayed after oral/topical exposure.
Media
- Elisha S, Heiner JS, Nagelhout JJ. Nurse Anesthesia. 7th ed. Elsevier; 2023.
References
- Elisha S, Heiner JS, Nagelhout JJ. Nurse Anesthesia. 7th ed. Elsevier; 2023.
Media Attributions
- sequence-of-events

