Bronchial Blockers
Bailey Freeman, DNP, CRNA and Angela Mordecai, DNP, CRNA
Quick Facts
- A bronchial blocker (BB) is a catheter with a balloon that is inserted through a standard endotracheal tube (ETT).
- The balloon can be inflated in either the left or right mainstem bronchus to achieve lung isolation.
- A BB can be used to isolate specific lobes when it is positioned in distal airways.
- Must use fiberoptic bronchoscope for placement.
Indications
Lung isolation methods optimize surgical access while maintaining one-lung ventilation (OLV):
- Provide motionless, accessible operative field.
- Prevent contralateral lung contamination from hemorrhagic/purulent material.
- Enable differential lung ventilation.
Specific Use Cases:
- Difficult airway requiring awake oro/nasotracheal intubation and OLV.
- Existing endotracheal/tracheostomy tube requiring OLV.
- Cases requiring postoperative mechanical ventilation (a DLT is not appropriate for postoperative mechanical ventilation).
Contraindications
- Cases requiring rapid lung isolation.
- Situations where DLT may be more appropriate.
Procedure
Equipment Needed:
- Appropriately sized Bronchial Blocker.
- Test balloon inflation/deflation and lubricate BB before insertion.
- Standard single-lumen ETT (7.5-8.0 mm ID for adults).
- Flexible fiberoptic bronchoscope.
- Multiport adapter (usually comes in BB package; attach to ETT).
- Back-up airway equipment.
Technique
For left-sided placement, rotate head toward right to align left mainstem bronchus.
- Establish endotracheal intubation.
- Attach multiport adapter.
- Perform initial bronchoscopy (verify 3-4 cm between ETT tip and carina).
- Guide BB into position under bronchoscopic visualization.
- Position BB 5-10 mm below carina.
- Test position with balloon inflation (5-8 mL air for adults).
OLV Initiation with a Bronchial Blocker in Place
- Administer 100% oxygen.
- Confirm BB position bronchoscopically.
- Stop positive pressure ventilation.
- Disconnect circuit and allow expiration.
- Inflate BB balloon under visualization.
- Apply intermittent suction.
- Resume ventilation on nonoperative side.
Confirmation Steps
- Verify BB exits ETT’s distal opening (not Murphy eye).
- Confirm proper balloon inflation (5-8 mL for most adult BBs).
- Reconfirm position after patient repositioning.
- Verify position in lateral decubitus position.
The clinician should also confirm:
- Adequate ventilation and isolation.
- Surgical field feedback.
Documentation Requirements
- BB type and size used.
- ETT size.
- Confirmation of position.
- Balloon inflation volume.
- Any complications.
SCOPE GUIDE
Strategies
Size Selection/Considerations
- Arndt® 7Fr: Use with 7.5mm ID ETT.
- Arndt® 9Fr: Use with 8.0mm ID ETT.
- Cohen® 9Fr: Use with 8.0mm ID ETT.
- EZ-Blocker® 7Fr: Use with 7.5-8.0mm ID ETT.
Device-Specific Notes:
- Arndt®: Remove wire guide after positioning.
- Cohen®: Use wheel-turning device for tip deflection.
- Uniblocker®: Hockey stick shape aids positioning.
- EZ-Blocker®: Y-shaped design seats on carina.
Clinical Optimization
Troubleshooting
- Dislodgment: Reconfirm position frequently, secure fixation, and ensure careful patient positioning.
- Inadequate seal: Adjust balloon inflation, check position relative to carina, verify appropriate size selection.
- Difficult placement: Use specific BB features, consider alternative BB type, ensure proper lubrication.
Patient Management
- Frequent position reconfirmation prevents dislodgment.
- Adjust balloon inflation volume for optimal seal.
- Utilize device-specific features for placement.
- Monitor position during patient movement.
- Address any hypoxia immediately when detected.
- Maintain clear, ongoing communication with the surgical team.
Quick Resources
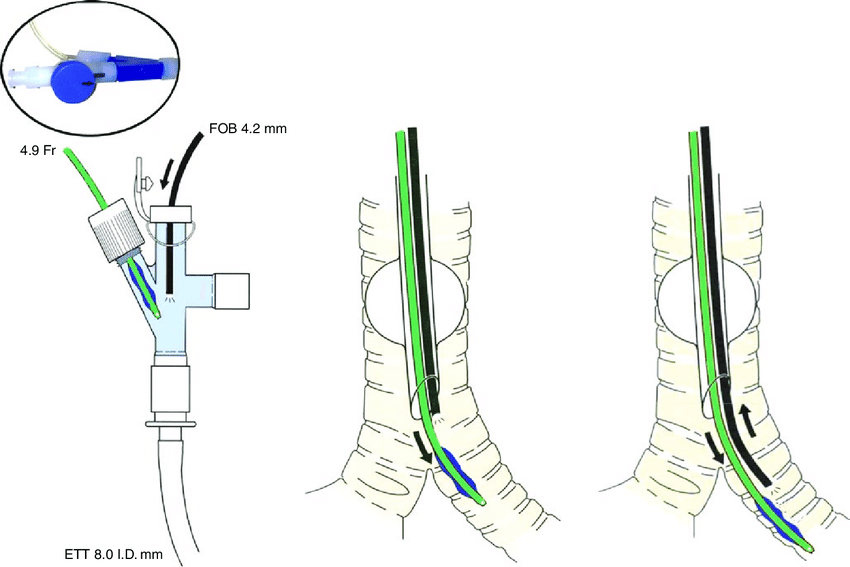
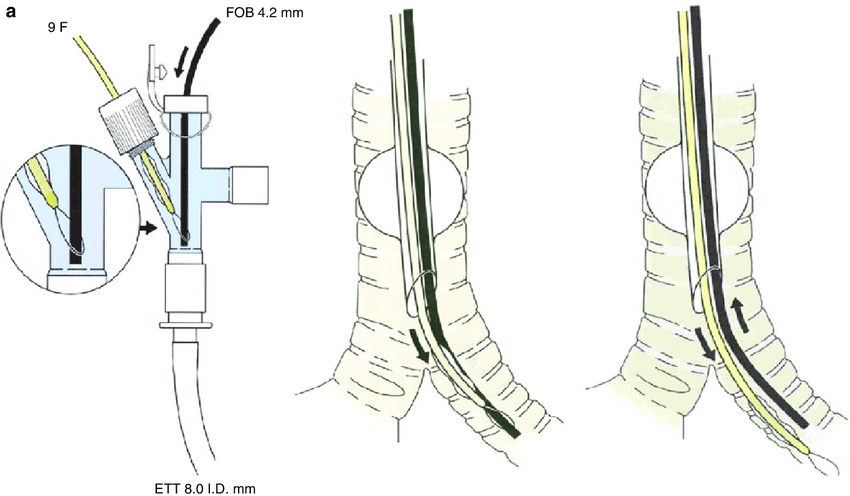
Source: Campos JH, 2019. Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].
(b) Optimal position of a bronchial blocker in the right or left mainstem bronchus as seen with a fiberoptic bronchoscope.
(A) Right mainstem blocker; (B) Left mainstem blocker.
Source: Campos JH, 2019. Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].
References
This work adapts content from FOAMed Medical Education Resources by LITFL (Life in the Fast Lane), licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original work can be found at https://litfl.com.
- Nickson C. Selective Lung Ventilation. Life in the Fast Lane. Published July 5, 2024. Accessed January 28, 2025. https://litfl.com/selective-lung-ventilation/
- Life in the Fast Lane. Double-lumen Endotracheal Tube (DLT). Published 2020. Updated 2024. Accessed January 28, 2025. https://litfl.com/double-lumen-endotracheal-tube-dlt/
- Campos JH. Separation of the lung: Double-lumen endotracheal tubes and endobronchial blocker. In: Cohen E (ed). Cohen’s Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 213-39.
- Campos JH. Lung isolation in patients with a difficult airway in thoracic anesthesia. In: Cohen E (ed). Cohen’s Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 240-8.
- Campos J. Lung isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. 2nd edition. Switzerland. Springer Nature. 2019: 283-309.
- Campos JH. Which device should be considered the best for lung isolation: Double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol. 2007; 20:27-31.
- Campos JH, Musselman ED, Hanada S, Ueda K. Lung isolation techniques in patients with early stage or long-term tracheostomy: A case series report of 70 cases and recommendations. J Cardiothorac Vasc Anesth. 2019; 33: 433-9.
Media Attributions
- The-Cohen-flexitip-bronchial-blocker-with-a-multiport-connector-90 © Campos JH, 2019. Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].
- a-Placement-of-an-Arndt-R-blocker-through-a-single-lumen-endotracheal-tube-with-the © Campos JH, 2019. Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].

