Epidural
Bailey Freeman, DNP, CRNA and Angela Mordecai, DNP, CRNA
Quick Facts
- An Epidural is a form of neuraxial anesthesia that provides a continuous infusion of local anesthetic into the epidural space, resulting in loss of pain sensation in the lower abdomen and lower extremities.
- The procedure involves the threading of a sterile catheter into the epidural space, where local anesthetic exerts its effects on the area surrounding the nerve roots.
- Adjunctive medications are often administered with the local anesthetic for a synergistic effect, providing additional analgesic benefits.
- Epidural blocks may be “dosed-up” with high potency local anesthetics to provide surgical anesthetic conditions. This is often performed if a laboring patient requires emergency cesarean delivery.
- Neuraxial anesthesia avoids systemic circulation of medications and allows for the mother to be awake for the birth.
- The patient may remain awake, or be sedated for anxiolysis.
- Epidurals allow for continuous infusion of medication, therefore the effects can last as long as the catheter is in place.
Indications
Epidural blocks are indicated for various surgical procedures and pain management:
- Cesarean section
- Thoracic surgery
- Abdominal surgery
- Lower limb surgery
- Post-operative pain control
- Analgesia for traumatic injury
- Rib fractures
- Pelvic fractures
- Lower extremity fractures
Absolute Contraindications
- Patient refusal
- Allergy to local anesthetic
- Infection at the site of placement
- Elevated intracranial pressure
- Severe coagulopathy
- Severe aortic stenosis
- Pre-existing spinal cord damage
Relative Contraindications
- History of spinal surgery
- Aortic stenosis
- Anticoagulants
- Certain neurological disorders
- Inability to maintain position for procedure
Procedure
Equipment Needed:
- Sterile epidural kit
- Local infiltration (1% Lidocaine)
- Test dose (1.5% Lidocaine w/Epinephrine)
- 25-gauge needle for skin infiltration
- 18-gauge blunt tip needle to draw up local anesthetic
- 9 cm Tuohy needle with stylet
- Loss of resistance (LOR) syringe
- Sterile saline
- Antiseptic skin solution
- Sterile epidural catheter
- Alligator clip
- Sterile syringes, gauze, sponges, and drape
- Mayo stand
- Sterile gloves
- Preservative-free local anesthetic (i.e. bupivacaine) for epidural infusion
- Epidural tubing
Technique [add video]
- Apply monitors (SpO₂ and NIBP)
- Assist patient in sitting neuraxial position
- Position patient on the side of the bed, rounding the back out in a “mad cat” or “shrimp” position
- Locate iliac crests and palpate vertebral interspaces
- Mark the intended insertion site (often L3–4 or L4–5)
- Prepare for procedure:
- Using sterile technique, open the epidural kit on the mayo stand or epidural cart
- Apply sterile gloves
- Clean the back with sterile betadine solution (allow drying time)
- Draw up 3 ml of 1% lidocaine and attach a 25g needle
- Draw up 5 ml of test dose
- Draw up saline into the loss of resistance syringe, leaving a bubble of airSaline is not necessary, but will prevent pneumocephalus if air is accidentally injected into the spinal space
- Place a sterile drape with an opening around the block placement site
Block placement
- Perform a local anesthetic skin wheel (with about 2 ml of 2% lidocaine) at the block placement site
- Introduce the Tuohy needle (initially 2.5–3 cm deep, possibly more with high BMI patients)
- Remove the stylet from the Tuohy needle
- Attach the loss of resistance syringe
- Advance slightly cephalad (depth will depend on patient size)
Typically, “loss of resistance” occurs around 3–9 cm, depending on the patient’s size - Always brace your left hand on the patient’s back to secure the needle position
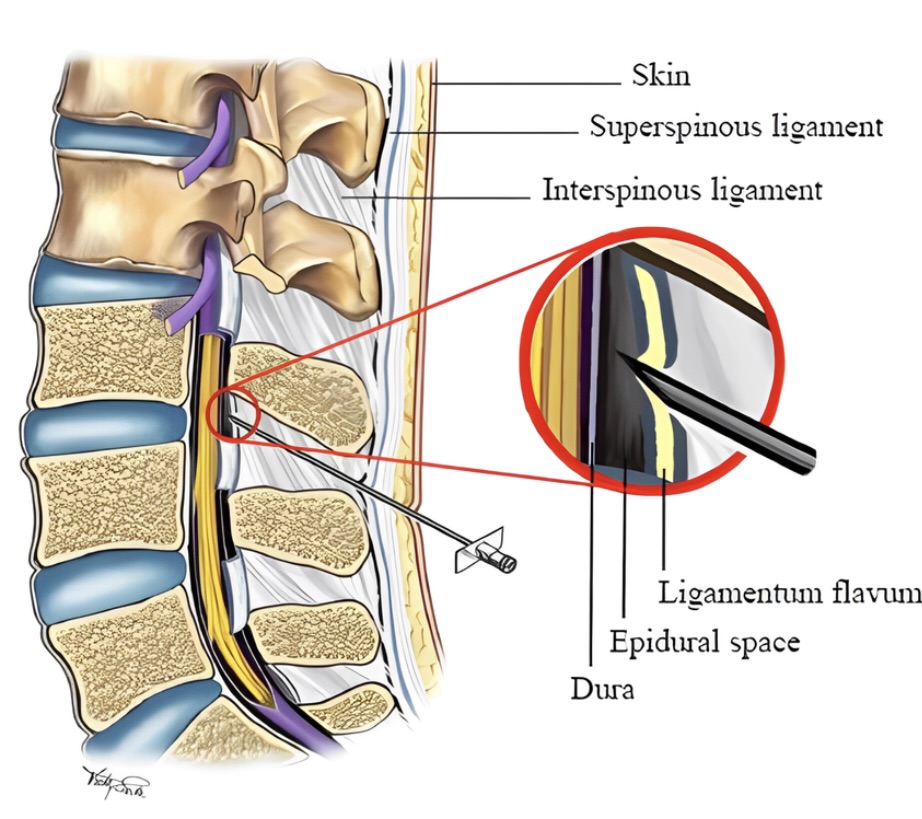
- Keep continuous pressure on the LOR syringe as you slowly advance through the layers of tissue:
- Subcutaneous tissue
- Supraspinous ligament
- Intraspinous ligament
- Ligamentum flavum “pop” *This is where we feel “loss of resistance”
- Once you feel the “pop” of the ligamentum flavum, do not advance any further as you are now in the epidural space
- The epidural space is considered a potential space; it will open with the injection of fluid
- Consider injecting the remaining saline from the LOR syringe to open the space
- Remove the LOR syringe, keeping the back of your left hand braced against the patient’s back while holding the Tuohy needle in place
DETERMINING DEPTH OF EPIDURAL SPACE
- Take note of the remaining cm marks on the needle
- Subtract the number of remaining cm’s (outside the skin) from 9 cm (total length of the Tuohy) to determine the cm depth of the epidural space
- Insert and advance the epidural catheter through the Tuohy needle, feeding it 3–5 cm past the depth of the Tuohy
TEST DOSING
- Carefully remove the Tuohy needle while keeping the catheter in place
- Attach an alligator clamp to the catheter
- Aspirate to assess for any blood or CSF in the catheter (if either is present, remove the catheter and start over at another level)
- Administer 2 cc of test dose [1.5% Lidocaine/1:200,000 epinephrine] and observe for signs of intravascular or subdural injection
- If no signs of intravascular or subdural injection are observed, proceed with the loading dose
- The loading dose is usually 5–10 cc of epidural infusion solution
- Depends on patient factors, labor status, height, provider preference
- Assist the patient into the supine position (with left uterine displacement if pregnant)
Confirmation Steps
- If the test dose is intravascular, the patient will experience tinnitus, a metallic taste in the mouth (effects of the local anesthetic), and increased HR and BP (effects of the epinephrine)
- If the test dose is subdural, the patient will experience extreme heaviness and immobility in the lower extremities
- Within a few minutes of the test dose, the patient may notice a warm/tingling sensation in their legs, as though they are “falling asleep.” This is a good sign that the epidural is working
- After 30 minutes, the epidural level should be at the level of the umbilicus (T10)
- “Testing” of the epidural level may be accomplished with a cold object such as an alcohol swab or ice cube
- Epidurals work by gravity, so side-lying positions will cause the medication to bathe the nerves on the dependent side
Documentation Requirements
- Epidural kit lot number and expiration date
- Sterile measures taken
- Patient position during and after block placement
- Level of block placement
- Number of attempts
- Needle types used
- Level of sensory blockade obtained
- Any complications
SCOPE GUIDE
Strategies
- Review patient labs, with particular attention to WBC count and platelet count, which may indicate infection or coagulopathy.
- Epidurals can be performed in the sitting or lateral side-lying positions
- Sitting is more common as it is easier to place midline.
- Patient must be educated on the procedure and required positioning.
- Patient must be able to maintain the necessary position, without moving during placement.
Clinical Optimization
- If patient on blood thinners, look to the neuraxial anticoagulant protocol to ensure appropriate timing has elapsed since the last dose.
- In anticipation of neuraxial-induced vasodilation, the patient should be fluid optimized prior to placement
- Administer 1 L of crystalloid; may also consider 250–500 ml colloid.
- Anxiolysis may be helpful in assisting the patient into position and remaining still
- This may be achieved with 2 mg IV midazolam or an IV narcotic.
- Note baseline vitals and ensure they are maintained within 20%.
- In the morbidly obese population, a longer Tuohy needle may be required to access the epidural space.
Pearls
- Have a trash can nearby to discard supplies such as betadine sponges.
- Before donning sterile gloves, elevate the table so that the insertion site is at chest-level.
- If having trouble getting into the epidural space, ensure positioning is correct.
- Patient may need to round out their back further to allow for maximal spreading of the spinous processes.
- Be sure to ask the patient if they feel the insertion pressure on one side or the other, as a slight offset from midline may direct the needle out of range.
- Generally, it is helpful to start at the lower end of the intervertebral space and advance slightly cephalad.
- If osseous matter is obstructing placement, pull back and redirect until the needle advances smoothly.
- Fentanyl or Precedex can help eliminate a “hot spot”
Complications
- Hypotension: due to reduction in SVR
- Neosynephrine and Ephedrine should be readily available.
- IV fluids should be infusing wide-open.
- Consider colloid infusion.
- Nausea/Vomiting:
- Sodium Bicitra should be given prior to block placement.
- Zofran (dose per provider discretion) given prior to, or shortly after, placement.
- Further antiemetics such as decadron, reglan, or phenergan per provider discretion.
- Unilateral Block:
- Patient may feel more numb on one side.
- Position the patient on the side that is less numb so that gravity can allow the local anesthetic to cover the nerves that aren’t numb.
- If unable to obtain adequate coverage with repositioning, assess the catheter to ensure it has not migrated deeper.
- May need to pull the catheter back slightly as the tip may favor one direction.
- High Spinal *EMERGENCY*: Patient will lose the ability to breathe
- This may occur if there was a “wet tap” or any breach in the dura.
- Support ventilation with bag/mask if not contraindicated.
- If the patient is pregnant or has a full stomach, perform RSI and intubate.
- Administer midazolam as soon as possible for anxiolysis.
- Patient will need to remain on the ventilator until respiratory effort resumes.
- Post-dural Puncture Headache (PDPH): May occur as a result of the dura being punctured (a “wet tap”)
- Symptoms may begin immediately or develop over 24–48 hours.
- The headache will worsen when upright and resolve when supine.
- Conservative therapy includes IV/PO hydration, bedrest, analgesics, and caffeine.
- An epidural blood patch is effective in up to 95% of patients.
- Keeping saline in the LOR syringe reduces the risk of PDPH in the event of a wet tap.
- Epidural Hematoma: Rare complication (<1:150,000), usually a complication of coagulopathy during placement. May result in permanent nerve injury.
- Prevention is the best measure—pay close attention to preoperative lab values.
- Refer to the neuraxial protocol for patients on anticoagulants.
- Treatment includes steroids and anti-inflammatories.
- Surgical decompression of the hematoma may be warranted in extreme situations.
- Meningitis/Infection:
- May progress to neurological injury; strict sterile technique should avoid this scenario.
- May be treated with antibiotics or antivirals, depending on the organism.
Quick Resources
References
1. Barash PG, Cullen BF, Stoelting RK, et al. Clinical Anesthesia. 8th ed. Wolters Kluwer; 2017.
2. Cerebral Palsy Caused by Anesthesia. MyCerebralPalsyChild.org. Published March 22, 2018. Accessed February 15, 2025.
Media Attributions
- A schematic of the lumbar spine anatomy during an epidural needle insertion procedure. is licensed under a CC BY (Attribution) license

