Double Lumen Endotracheal Tubes
Bailey Freeman, DNP, CRNA and Angela Mordecai, DNP, CRNA
Quick Facts
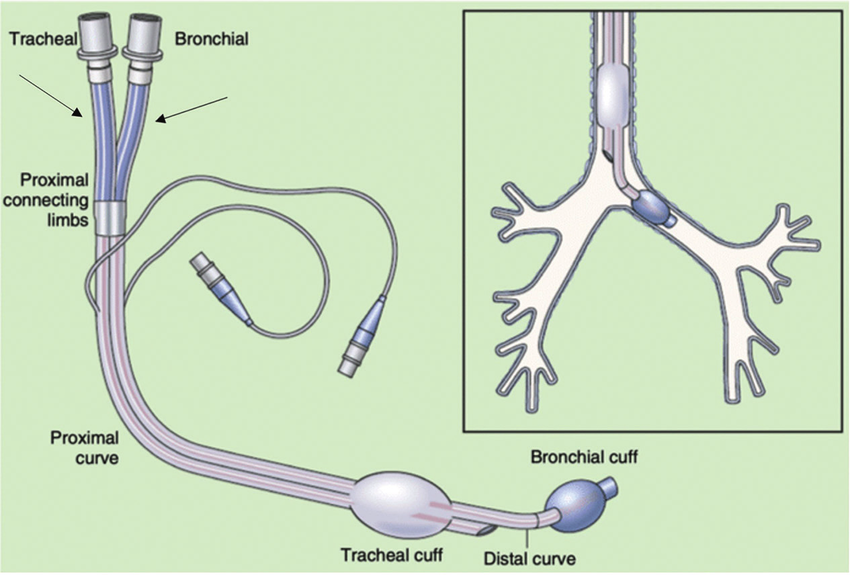
- Double-lumen endotracheal tubes (DLT) are used for lung isolation and one-lung ventilation (OLV).
- Two parallel lumens: one for the trachea and one for a main bronchus (left or right).
- Left-sided DLT are more commonly used than right-sided DLT.
- May be used to isolate either the left or the right lung.
- Right-sided DLT are designed with a special port to ventilate the right upper lobe.
- Proper positioning is critical; misalignment of tube can prevent ventilation to the right upper lobe (RUL).
- Used for: left-sided pneumonectomy, sleeve resection, or when left mainstem bronchus is compressed/distorted.
Indications
Lung isolation may be used in patients undergoing thoracic, esophageal, cardiac, vascular, or spine surgery to optimize surgical access while maintaining one-lung ventilation (OLV).
- Provide motionless, accessible operative field.
- Prevent contralateral lung contamination from hemorrhagic/purulent material.
- Enable differential lung ventilation.
Contraindications
- Difficult airways (consider Bronchial Blocker instead).
- Full-stomach patients.
- Emergency/rapid intubation scenarios.
Procedure
Equipment Needed:
- Appropriately sized DLT (For details on size selection, see SCOPe Guide).
- Direct or video laryngoscope.
- Flexible fiberoptic bronchoscope (small diameter).
- Lubricated stylet (goes in endobronchial lumen).
- Soft-tipped clamp.
- Assembled Y-connector (included in the DLT package).
- Backup airway equipment in case of difficult placement.
Technique
Blind Technique
- Perform laryngoscopy (direct or video).
- Gently insert tube with bronchial lumen facing patient’s toes (bronchial lumen concavity facing anteriorly).
- Pause at level of vocal cords.
- Advance endobronchial cuff just past the vocal cords, then remove the stylet.
- Turn DLT 90 degrees to left (or right, if right-sided) as you advance.
- Continue to advance tube into trachea so that tracheal cuff passes vocal cords.
- Advance DLT to approximately 29 cm depth at teeth for patients ≥170 cm, or when resistance is met.
- Inflate tracheal cuff and ensure bilateral lung ventilation.
- Inflate bronchial cuff to approximately 3ml, or minimal air to seal.
- Ensure that each lung can be isolated. Clamp appropriate lumen at Y connector/open port to air.
Bronchoscopy Guided Technique
- Lubricate fiberoptic bronchoscope.
- Thread DLT (endobronchial lumen) onto bronchoscope.
- Pass DLT through vocal cords under direct visualization.
- Guide to appropriate bronchus under direct visualization.
Confirmation Steps
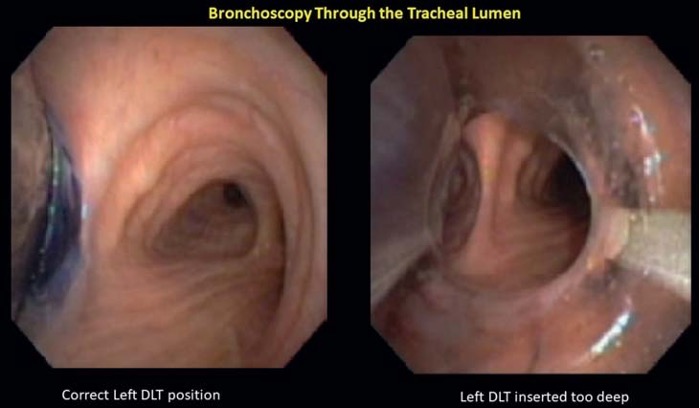
Confirm placement with fiberoptic bronchoscope both immediately after placement & after positioning.
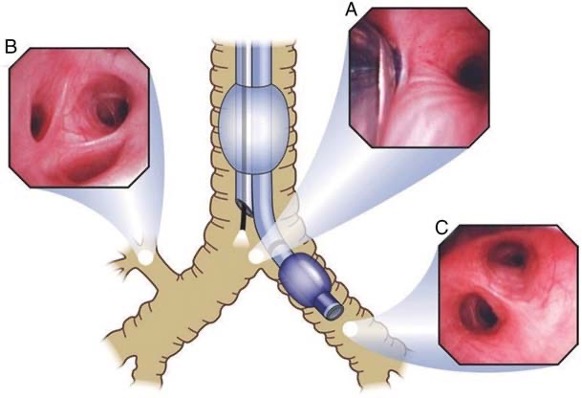
Confirmation (Left DLT)
- Insert scope through tracheal lumen:
- Should see fully inflated bronchial cuff located at least 5 to 10 mm below the carina inside the left mainstem bronchus.
- Ensure that bronchial cuff is not herniated out of the bronchus.
- Insert scope through bronchial lumen:
- Should see entrances to left upper and lower lobe bronchi.
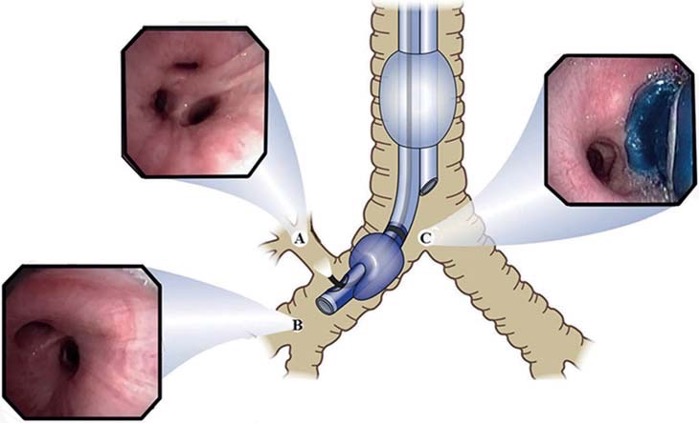
Confirmation (Right DLT)
- Insert scope through the tracheal lumen:
- Should see inflated endobronchial cuff just below the tracheal carina.
- Identify the entrance of the right main bronchus and right upper lobe bronchus.
Documentation Requirements
- DLT size used.
- Placement technique.
- Confirmation method.
- Any complications.
- Cuff volumes (tracheal and bronchial).
SCOPE GUIDE
Strategies
- Early recognition of malposition.
- Regular reassessment of ventilation throughout case.
- Clear communication with surgical team.
- Backup airway plan.
- Choose proper size DLT.
Size Selection/Considerations
- Height/sex-based selection:
- Females: 35-37 Fr.
- Males: 39-41 Fr.
- Consider individual variations based on:
- Extremes of height.
- Tracheal/bronchial diameter: radiological studies or ultrasound measurements.
- Previous airway interventions.
Clinical Optimization
Troubleshooting
- Insertion difficulties
- Use bronchoscope guidance.
- Consider bougie technique.
- Use a lubricated stylet.
- Lightly lubricate DLT.
- Optimize positioning.
- Once tracheal cuff is past the vocal cords, rotate DLT towards bronchus that is to be cannulated, turn patient’s head to opposite side to more easily advance DLT.
- Inadequate lung isolation
- Use suction catheter (usually included in DLT package) to more quickly/more completely deflate lung if needed.
- Verify position of DLT.
Pearls
Preparation
- Keep fiberoptic bronchoscope immediately available.
- Create and maintain organized equipment setup.
- Complete equipment checks before starting.
- Have backup airway devices ready and accessible.
Technical Considerations
- Secure DLT with tape to prevent any movement.
- For lung isolation: clamp the ADAPTOR, never the tube itself.
- During maintenance phase:
- Reduce pressure in the 3cc endobronchial cuff.
- This reduces airway trauma risk.
- Lung isolation maintains as air follows path of least resistance.
- Reduce pressure in the 3cc endobronchial cuff.
- Know that in emergencies, a standard ETT can be advanced into the target lung.
Management
- Never use 100% oxygen in patients with prior bleomycin exposure.
- Verify DLT position regularly throughout the case.
- Address any hypoxia immediately when detected.
- Maintain clear, ongoing communication with the surgical team.
Monitoring
- Combine clinical assessment with bronchoscopic visualization.
- Pay attention to subtle position changes.
- Stay ahead of potential complications.
- Watch the surgical field for feedback about positioning.
Quick Resources
![Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].](https://txwes.pressbooks.pub/app/uploads/sites/36/2025/02/a-Sheridan-right-sided-DLT-b-Mallinckrodt-right-sided-DLT-c-View-of-the-right-757x1024.png)
![Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].](https://txwes.pressbooks.pub/app/uploads/sites/36/2025/02/Displays-the-external-and-internal-diameters-of-the-differ-ent-sizes-of-DLTs-and-the.png)
References
This work adapts content from FOAMed Medical Education Resources by LITFL (Life in the Fast Lane), licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The original work can be found at https://litfl.com.
- Nickson C. Selective Lung Ventilation. Life in the Fast Lane. Published July 5, 2024. Accessed January 28, 2025. https://litfl.com/selective-lung-ventilation/
- Life in the Fast Lane. Double-lumen Endotracheal Tube (DLT). Published 2020. Updated 2024. Accessed January 28, 2025. https://litfl.com/double-lumen-endotracheal-tube-dlt/
- Campos JH. Separation of the lung: Double-lumen endotracheal tubes and endobronchial blocker. In: Cohen E (ed). Cohen’s Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 213-39.
- Campos JH. Lung isolation in patients with a difficult airway in thoracic anesthesia. In: Cohen E (ed). Cohen’s Comprehensive Thoracic Anesthesia. 1st edition. Philadelphia, PA. Elsevier. 2022: 240-8.
- Campos J. Lung isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. 2nd edition. Switzerland. Springer Nature. 2019: 283-309.
- Campos JH. Which device should be considered the best for lung isolation: Double-lumen endotracheal tube versus bronchial blockers. Curr Opin Anaesthesiol. 2007; 20:27-31.
- Campos JH, Musselman ED, Hanada S, Ueda K. Lung isolation techniques in patients with early stage or long-term tracheostomy: A case series report of 70 cases and recommendations. J Cardiothorac Vasc Anesth. 2019; 33: 433-9.
Media Attributions
- Typical-double-lumen-tube-DLT-and-appropriate-positioning-within-the-trachea-and.ppm © Updates in Anesthesia – The Operating Room and Beyond [Working Title]. October 2022. DOI: 10.5772/intechopen.107468. Licensed under CC BY 3.0.
- Leftsided © Used with permission from Campos JH.3
- Rightsided © Used with permission from Campos JH.3
- Bronchthrutrachea © With Permission from Campos JH.2
- a-Sheridan-right-sided-DLT-b-Mallinckrodt-right-sided-DLT-c-View-of-the-right © Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].
- Displays-the-external-and-internal-diameters-of-the-differ-ent-sizes-of-DLTs-and-the © Reproduced with permission from Campos JH. Lung Isolation. In: Slinger P (ed). Principles and Practice of Anesthesia for Thoracic Surgery. Springer Nature Switzerland AG; 2019. [DOI: 10.1007/978-3-030-00859-8_16].

