Central Venous Catheters
Bailey Freeman, DNP, CRNA and Angela Mordecai, DNP, CRNA
Quick Facts
- Real-time ultrasound guidance recommended to reduce complications; this is the technique we will focus on in this guide.
- Requires thorough anatomical knowledge and technical proficiency.
- Purpose:
- Measure central venous pressure
- Stable access for continuous drug administration
- Direct medication/fluid delivery to heart
- Common placement locations:
- Internal jugular vein (neck)
- Subclavian vein (below collarbone)
- Femoral vein (groin)
- PICC line (arm)
Indications
Central venous catheterization is indicated for:
- Securing a stable route for continuous or long term IV therapy administration
- Central venous pressure monitoring
- Emergency volume resuscitation
Absolute Contraindications
- Local infection at the insertion site
- Known thrombosis in the target vessel
- Active bleeding diathesis without correction
Relative Contraindications
- Severe coagulopathy (platelets <50,000/ml³, INR >1.8)
- Anatomical distortion
- Patient unable to remain still
Procedure
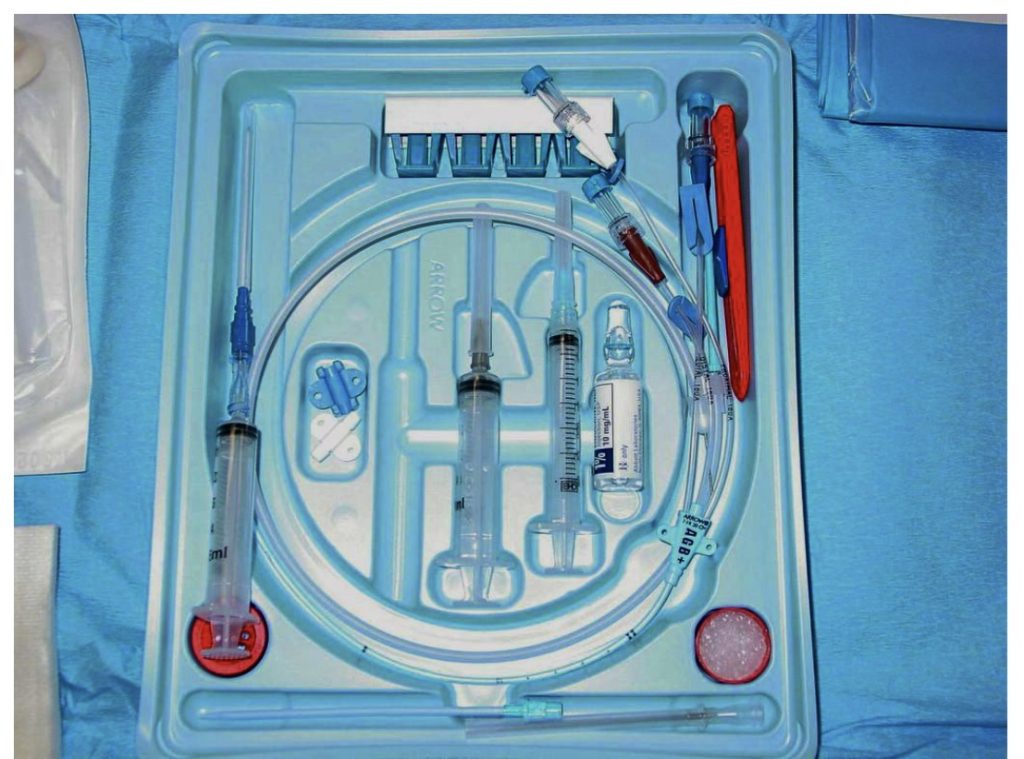
Equipment Needed:
- Ultrasound machine with high-frequency linear probe
- Central line kit (Seldinger technique)
- Sterile barrier equipment:
- Cap, mask, sterile gown
- Sterile gloves
- Large sterile drapes
- 1% chlorhexidine-alcohol or povidone-iodine
- Emergency cart accessible
Universal Procedure Steps
PRE-PROCEDURE
- Timeout verification
- Position patient appropriately
- Initial ultrasound survey
- Hand hygiene and donning PPE
- Chlorhexidine prep (≥90 sec) or Betadine (≥3 min)
- Sterile draping
- Equipment organization and port flushing
ACCESS
- US-guided vessel puncture with continuous aspiration
- Venous confirmation (multiple methods)
- Guidewire threading under ECG (max 15 cm)
- Skin nick (0.5 cm longitudinal)
- Tract dilation
- Catheter insertion
- Securing and dressing
CONFIRMATION STEPS
- Blood color/flow assessment
- Pressure manometry (3–10 cm H₂O for veins)
- Blood gas if needed
- Ultrasound visualization
- Chest X-ray verification
Site-Specific Considerations
INTERNAL JUGULAR (IJ)
Anatomy
- Location: Sedillot’s Triangle apex
- Depth: 1–2 cm
- Vessel characteristics:
- Oval-shaped, compressible
- Lateral and superficial to the carotid
- Key landmarks:
- Mandible angle
- SCM heads (sternal/clavicular)
- Thyroid cartilage
- Trachea
Technical Details
- Position:
- Trendelenburg 10–20° (increases diameter by 20–25%)
- Head rotation 15–30°
- Needle approach:
- 30–45° toward ipsilateral nipple
- Bevel up
- Continuous aspiration
- Ultrasound:
- Short axis for initial survey
- Long axis for wire confirmation
- Gel applied on both sides of the probe cover
- Coordinate probe movement with needle
Side Selection
- Right preferred:
- Direct SVC route
- Typically larger vessel
- Lower complication risk
- Left considerations:
- Difficult brachiocephalic angle
- Higher SVC perforation risk
- Thoracic duct risk (~2 L chyle/day)
SUBCLAVIAN
Anatomy
- Location: Behind the clavicle, above the first rib
- Becomes the axillary vein after the first rib
- Landmarks:
- Clavicle midpoint
- Deltopectoral groove
- Sternal notch
- SCM
Technical Approach
- Infraclavicular technique:
- Entry 1–2 cm below clavicle midpoint
- 10–15° toward the sternal notch
- Head neutral
- Trendelenburg for air embolism prevention
- Ultrasound guidance:
- View above/below the clavicle
- Track from the deltopectoral groove
- Can use in-plane or out-of-plane technique
- Clavicle positioned at screen edge for long-axis visualization
Special Considerations
- Highest pneumothorax risk
- Non-compressible site
- Avoid in coagulopathy
- Risk of pinch-off syndrome
- More comfortable for long-term use than IJ
FEMORAL
Anatomy
- NAVL sequence: Nerve, Artery, Vein, Lymphatics
- Entry: 1–2 cm below the inguinal ligament
- Position: Medial to the arterial pulse
- Depth: 2–4 cm typical
Emergency Access
- Common CPR choice
- Caution: Pulse may be venous during CPR
- Depth: 15–30 cm for IVC placement
Confirmation Methods
PRESSURE MANOMETRY TECHNIQUE
- Remove introducer needle
- Thread angiocath over the guidewire
- Remove the guidewire
- Attach extension tubing
- Allow 2/3 fill with blood
- Elevate the tubing straight up
- Assess height (3–10 cm = venous)
X-RAY ASSESSMENT
- Anatomic landmarks:
- Heart ≤50% of thoracic cavity
- Trachea midline
- Lungs appear black/air-filled
- Right hemidiaphragm elevated
- Tip position:
- Above pericardial reflection
- 0.5–1 cm below the carina
- T4–T6 vertebrae
- Target lengths:
- Right IJ: 16 cm
- Right SC: 18 cm
- Left SC: 21 cm
- Left IJ: 19 cm
Documentation Requirements
- Procedure timeout completion
- Use of ultrasound guidance
- Catheter type and size
- Number of attempts
- Confirmation methods used
- Final catheter tip position
- Any complications
SCOPE GUIDE
Strategies & Clinical Optimization
CVC Complications Management: Risk Assessment
- Body habitus
- BMI >30 or <20
- Anatomical variants
- Uncontrolled movement
- Medical conditions
- Coagulopathy
- Local infection/burns
- Hypovolemia
- History
- Previous catheterization
- Prior radiotherapy
Technical Factors
- Operator experience
- Multiple needle passes
- Large catheter size
- Positioning issues
- Inadequate sterile technique
- Suboptimal ultrasound usage
Prevention Protocol
Pre-Procedure
- Ultrasound mapping
- Risk factor identification
- Equipment verification
- Optimal patient positioning
- Sterile barrier preparation
During Procedure
- Real-time ultrasound guidance
- Limited attempts (≤3)
- Continuous needle visualization
- Wire control maintenance
- ECG monitoring
- Sequential safety checks
Complications Recognition & Management
Immediate Complications
- Vascular
- Arterial puncture
- Air/thrombus embolism
- Hematoma
- Cardiac
- Arrhythmias (risk >18 cm depth)
- Cardiac perforation/tamponade
- Pulmonary
- Pneumothorax
- Hemothorax
- Hydrothorax
- Neural
- Nerve injury
- Thoracic duct injury (left side)
Delayed Complications
- Infectious
- Central line bloodstream infection (2.4–5% rate)
- Cellulitis
- Financial impact: $34,000–56,000 per infection
- Mechanical
- Thrombosis
- Catheter migration
- Position-related issues
High-Risk Scenarios
- Coagulopathy with subclavian approach
- Non-compressible vessels
- Emergency placement during CPR
- Previously irradiated sites
- Complex anatomy
Pearls
- Always visualize needle tip during insertion
- Never force guidewire advancement
- Stop if resistance is felt during dilation
- Use pressure transduction or blood gas when in doubt
- Confirm venous placement before dilation
- Maximum of 3 attempts before seeking assistance
IJ Access
- Contract neck to identify SCM
- Shoulder towel roll helps landmark identification
- Long-axis visualization for guidewire
- Left lung dome higher – increased pneumothorax risk
Subclavian Access
- Longitudinal/sagittal view orientation
- Vein becomes axillary after first rib
- More comfortable long-term than IJ
- Highest pneumothorax risk
- Non-compressible site
Femoral Access
- Emergency/CPR scenario choice
- Verify venous vs. arterial pulse during CPR
- Higher infection risk than other sites
- Useful when upper body access contraindicated
Quick Resources
Key Measurements
- IJV depth from skin: ~1–2 cm
- Optimal Trendelenburg: 10–20°
- Time for site pressure: 10 min
- Dressing change intervals: 2 days (gauze), 7 days (transparent)
Key Images/Diagrams
Anatomical Views
- Sedillot’s triangle anatomy
- IJV relationship to carotid
- Cross-sectional vessel anatomy
- Wire and catheter positioning
Critical Angles
- Needle approach views
- Ultrasound probe positioning
- Guide wire advancement angles
- Head rotation limitations
References
1. Safety Committee of Japanese Society of Anesthesiologists. Practical guide for safe central venous catheterization and management 2017. J Anesth. 2020;34(2):167-186. doi:10.1007/s00540-019-02702-9
Media Attributions
- CVC Kit is licensed under a CC BY-SA (Attribution ShareAlike) license

